In 1998 The Women’s Health and Cancer Rights Act (WHCRA) was put into place as a federal law to protect a patient's right to choose breast reconstruction in connection with a mastectomy; this is now at risk as per the most recent attack on women’s healthcare and benefits as put forth by the Centers for Medicare and Medicaid Services (CMS) recommendation to collapse surgery codes into one simplified billing bucket, therefore, forcing patients to choose treatment paths that may not be best for them. “When you don’t have an option, you don’t have a choice.” Says Elisabeth Potter, MD of breast reconstruction and plastic surgery based out of Austin, Texas. Dr. Potter has performed thousands of DIEP flap procedures, typically performing 250 surgeries a year through insurance to patients around the country.

What is a DIEP flap vs a TRAM flap?
Why would patients choose a DIEP flap surgery?
Patients have many options when it comes to choosing the breast reconstructive procedure that is right for them and their treatment. Patients have the choice to remain flat following mastectomy surgery, they can rebuild the missing breasts with implants, or they can opt to use their tissue to restore the breast mounds that are now missing. Each of these options requires different expertise and access from the other, and in most cases, are not only a treatment option but a personal choice for what suits the patients' lifestyle and desired outcome the best. Not every patient is a candidate for each option, and each option comes with its own list of side effects and challenges.
When is a DIEP flap surgery the better option for breast reconstruction?
Depending on a person’s diagnosis and treatment path, a DIEP flap may be the better choice when opting for breast reconstruction. Some patients will weigh the growing concerns of using a foreign object in their bodies, such as implant reconstruction. About 20% of breast reconstructive surgeries are DIEP flap surgeries which last a lifetime, compared to implant reconstruction using a medical device that does not last a lifetime and requires multiple additional surgeries, which can lead to additional complications over time, and lifelong imaging for maintenance. Additional concerns can range from the increase in BIA-ALCL (Breast Implant Associated Lymphoma) to BII (Breast Implant Illness), which led the FDA to approve a “Black Box” warning on the manufacturing of implants to warn patients of the risks. Patients that face advanced breast cancer may require radiation as a form of their treatment. Implant-based reconstruction has a very high surgical complication rate compared to autologous reconstruction.
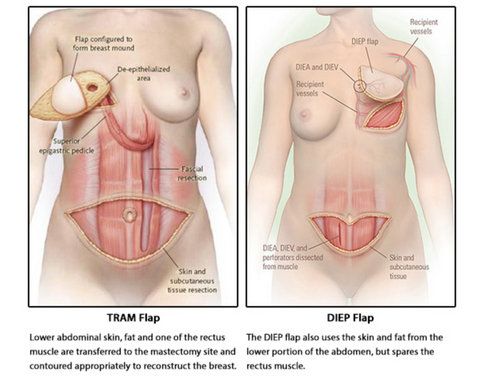
The DIEP flap leaves the abdominal muscle intact, strong, and health, saving function of the internal muscle structure and helps patients return to life quicker without the lifelong disabilities and weakness that TRAM procedures often cause. DIEP uses microsurgical techniques that get patients out of the hospital sooner, which leads to a decrease in the use of pain medications, and high costs for long hospital stays. Once the tissue has healed, very few cases need additional surgeries. This is not the case with implant reconstruction, as many patients require revisions and are often recommended to replace the internal device every 10-15 years.
Why would a shift in billing codes limit exposure to DIEP flap procedures?
DIEP flap microsurgery is the foundation of modern breast reconstruction. The availability of DIEP flap means that women who want or need natural breast reconstruction don’t have to sacrifice their strength. They can continue living active lives, thriving in their bodies. Women facing breast cancer who once underwent muscle removing surgeries like the TRAM flap experienced lifelong negative side effects like significant permanent weakness and hernia formation.
Surgeons must be allowed to perform and bill for DIEP flaps with transparency. If surgeons are not reimbursed for these advanced procedures, as they have been until now, access to these procedures will be severely limited. Microsurgery may very well be one of the most complicated forms of breast reconstruction to date; however, punishing patients by not allowing surgeons to bill as required for the additional time in operating rooms required to perform such a procedure is not the answer. There is only one answer, and that is patients WILL suffer. This update to billing codes will impact community-driven plastic surgeons (those that reside outside academic centers) and limit access to patients nationwide. Many patients do not live in metropolitan areas that have large institutions for treatment that require hours of driving to get to appointments, treatments, and surgeries. By limiting the codes and reducing medical reimbursement, smaller practices would be unable to perform these surgeries for the required costs. As a breast cancer community patient, I talk directly about the limitations in treatment and care when seeking out plastic surgeons who can perform the best surgery for us and our bodies. Many have already stopped performing tissue-based breast reconstruction due to poor reimbursements, denials, and extensive pressures on overhead and procedural times. This is not ok. When reconstruction options are unavailable for patients, they are forced into decisions they wouldn’t otherwise have made. This will also broadly impact our underserved and underinsured communities, especially and patients of color as they already face many barriers for equal and accessible care they deserve, and this will just add another barrier to treatment and care that is best for any patient.

How you can help?
- IF you have undergone a DIEP flap procedure, write to your local representatives sharing your personal story on why this procedure was important to you and your treatment.
- IF you have not undergone a DIEP flap but believe all patients diagnosed with breast cancer should have the right to choose their reconstructive surgery, write them. ASK them to sign the bill.
- IF you are interested in women’s health care and equality, write your local congresspeople to address the importance of access and availability to surgery options following a cancer diagnosis. ASK them to sign the bill.
We urge you all to take action, as this is just one step into a very deep and dark place that will continue to limit access and coverage for reconstructive procedures after a cancer diagnosis, as CMS has proven it’s intention to restrict access to the appropriate care required to live a full life following a cancer diagnosis..
1 in 8 women will be diagnosed in their lifetime. They should have a right to choose the BEST option for their treatment and overall well-being following a diagnosis, just as the Women’s Health and Cancer Rights Act addressed so clearly in 1998. We cannot turn back the hands of time and limit access to those of us living and facing this debilitating diagnosis.
Visit Dr. Potter Reconstructive Surgery to learn more about DIEP flap procedures and hear from her patient, Deborah, about her first hand experience and why she chose DIEP flap after breast reconstruction. Tune in HERE.
FIND YOUR LOCAL REPRESENTATIVE – CLICK HERE

If you need help writing a letter, please click here to use our sample letter as a guide.










